Astounding: Unmasks Exclusive Surgical Insights by Gough Surgical, PLLC!
Planet TV Studios reveals a film feature about Dr. Brandon Gough's Cutting-edge Surgical Developments in "New Frontiers" — Airing the spring of 2024 on National Broadcast and Video On-Demand.
BOCA RATON, FL, USA, March 5, 2024 / ReportWire.org -- Planet TV Studios rolls out its new broadcast series, "New Frontiers," highlighting the trailblazing successes by Gough Surgical, PLLC. This series uncovers the forward-thinking advancements steered by Dr. Brandon Gough, M.D., an eminent musculoskeletal surgeon specializing in state-of-the-art microinvasive strategies coupled with robotic surgery for hip and knee replacements.
"New Frontiers" constitutes an absorbing probe thoughtfully assembled designed to reveal cutting-edge establishments defining the next generation of healthcare worldwide. Set your reminder for the sequential documentary releases broadcast during the mid-2024 period via countrywide TV channels, Bloomberg TV, and conveniently streamable on digital platforms Amazon online, Google Play Video, Roku, and more.
Planet TV Studios is thrilled to welcome Gina Grad as the primary presenter. Gina is a renowned literary figure, podcast presenter, and seasoned radio professional based in Los Angeles, California. Her previous experience includes being sharing the role of co-host and news anchor on the Adam Carolla Show, a podcast famous for its Guinness World Record in episode downloads. Gina has additionally been an anchor at KFI 640 AM and spearheaded morning shows on 100.3 FM. She is now leading "The Bryan and Gina Show, The Official Podcast of LA Magazine." In parallel with her broadcast endeavors, she authored "My Extra Mom," a narrative designed to guide kids and stepparents in navigating the difficulties encountered in blended family setups.
Dr. Brandon Gough, M.D., is acknowledged as a notably acclaimed orthopedic surgeon, board-certified and widely recognized for his mastery in arthroplasty of the hip and knee inside Phoenix, Arizona. Employing state-of-the-art robotic technology alongside modern micro-invasive procedures and muscle-sparing methods, Dr. Gough is dedicated to facilitating swift returns to dynamic lives for his patients after surgery. His focus on maintaining soft tissue integrity ensures faster healing, minimizes inpatient duration and in select cases permits outpatient joint replacement. He is acclaimed as a worldwide authority in the Direct Superior Approach complemented by muscle-sparing robotic techniques.
Education stands as a cornerstone for Dr. Gough, recognizing its pivotal role in providing top-notch patient care through staying abreast of advancements in Orthopedic Medicine. Upon finishing his undergraduate education at Spring Hill College situated in Mobile, Alabama, he advanced to earn his medical degree at Creighton University School of Medicine located in Omaha, Nebraska. Dr. Gough deepened his practical knowledge through residency and internship in General Orthopedics at the University of Kansas, School of Medicine situated in Wichita, Kansas, and was honored as the Resident Teacher of the Year. He undertook further specialized training through a fellowship in Lower Extremity Adult Reconstruction at the Arizona Institute of Bone and Joint Disorders.
Being board-certified by the American Board of Orthopedic Surgeons and actively involved with organizations like the American Academy of Orthopedic Surgeons (AAOS), Dr. Gough's commitment to excellence extends beyond his practice. He functions as Vice President of the Orthopedic Surgery Interest Group and upholds his memberships in the American Medical Association and American College of Physicians. He practices at the distinguished Orthopedic Institute of the West—where he played a role in its establishment—and holds surgical privileges at Scottsdale Abrazo Hospital, Liberty Hospital, and other select centers in the Phoenix/Scottsdale, AZ region. Driven by his passion for evolving surgical practices, he champions the establishment of a robotic hip and knee replacement center of excellence while imparting his expertise to surgeons around the world.
Alongside his medical practice, Dr. Gough persistently devotes himself to community engagement, offering volunteer services to organizations such as the Magis Clinic, Madonna School, Habitat for Humanity, and Sienna St. Francis Clinic.
Remarkably, his consultant and educational role with Zimmer Biomet strengthens his commitment to the evolution of orthopedic practices and surgical methods.
Planet TV Studios is: Planet TV Studios produces groundbreaking, real-life TV series that present expert updates on important business, medical, and socially responsible matters.
For more information about Gough Surgical, PLLC, please visit https://goughmd.com.
For more information about the series, please visit https://planettvstudios.com / https://planettvstudios.com/backstage/ or contact Christian Alain at 888-210-4292 x100 or email christian@planettvstudios.com.
Gough Surgical Adult Hip & Knee: Pioneering subsequent period in Orthopedic Medicine
Amid the landscape of bone and joint surgery, accuracy, know-how, and creativity come together at Gough Surgical Adult Hip & Knee, a renowned clinic devoted only to hip and knee arthroplasty for adults.
Under the authoritative command of Dr. James Gough, this focused clinic has received widespread praise for revolutionizing patient experiences by regaining motion, mitigating suffering, and remarkably uplifting life standards for a multitude of patients.
Creating New Yardsticks in Skeletal Surgery
Orthopaedic interventions, specifically related to hip and knee operations, constitute the widely practiced interventions executed across the globe.
Yet, the success statistics and patient experience ratings are markedly different as determined by operative skill, facility quality, and the method of the surgeon.
Gough Surgical separates itself by focusing exclusively on adult hip and knee replacements, providing intensive expertise uncommon in the general field.
Dr. James Gough, celebrated for his operative exactness and empathetic care, has dedicated his career to mastering these complex procedures.
His clinic, Gough Surgical Adult Hip & Knee, well-located to serve a diverse patient base, has come to represent excellent clinical results, prompt recoveries, and improved patient experience.
Merit Derived from Specialization
What compels the focus on only adult hip and knee procedures?
Dr. Gough asserts that, concentrated practice engenders incomparable expertise.
"By focusing solely on adult hip and knee replacements, we've developed an unparalleled level of proficiency," remarks Dr. Gough.
This specialist knowledge leads to minimized complications, diminished operative risks, and improved clinical experiences.
Innovative Surgical Methods and Equipment
Gough Surgical Adult Hip & Knee systematically applies state-of-the-art technology to elevate procedural precision and clinical results.
One of the prominent aspects of the clinic entails employing advanced robotic operative systems.
These innovative technologies support extraordinary exactness, culminating in refined prosthetic placement adapted to the unique anatomy of each patient.
"Robotic assistance doesn't replace the surgeon's expertise—it enhances it," asserts Dr. Gough.
Personalized Care: Exceeding Mere Procedures
At Gough Surgical, patient attention is not limited to the operating table.
From initial consultation through thorough post-operative evaluations, personalized care is provided continuously to every patient.
This integrated method secures physical recuperation and fosters emotional comfort and confidence throughout the healing journey.
Dr. Gough reminds us, "Acknowledging every patient's individual needs, insecurities, and goals is indispensable." Specialized care notably boosts recovery success and patient contentment.
All-Encompassing Pre- and Post-Surgical Assistance
Gough Surgical’s focus on holistic patient support manifests through its detailed pre-surgical planning and meticulous post-surgery monitoring programs.
Customized pre-surgical classes, in-depth patient seminars, and face-to-face consultations prepare patients physically and mentally, lowering stress and spurring informed choices.
Subsequent to surgery, the clinic’s regimented recovery plans and bespoke physiotherapy schedules support accelerated, smoother recuperations.
Clients admire the lucid guidance, frequent progress assessments, and readily available professional support, notably augmenting their recovery experience.
Progressive Solutions for Difficult Conditions
Gough Surgical Adult Hip & Knee specializes in managing multifaceted conditions that other practices might deem difficult.
Spanning from multifaceted joint reoperations to managing critical arthritis conditions, the clinic supplies groundbreaking interventions with expert surgical techniques, minimally invasive procedures, and personalized implant systems.
These innovative therapies regularly contribute to brisker healing, lowered surgical pain, and reestablished functionality, allowing individuals to return to vibrant, pain-free living with speed.
A Heritage of Client Contentment
The patient stories attest to the remarkable improvements achieved through its treatments.
Patients commonly report reclaiming independence, experiencing substantial pain relief, and enjoying a superior quality of life following their operations.
"Walking without pain was something I never imagined possible again," notes Mary Thompson, a recipient of a full knee replacement at Gough Surgical.
"Dr. Gough and his team didn't just restore my knee—they gave me my life back," continues Mary Thompson.
Research and Continued Education
Beyond surgical mastery, Gough Surgical Adult Hip & Knee actively fuels advancements in orthopedic care with continuous research and training.
Dr. Gough frequently contributes to clinical research, delivering key data that improves orthopedic practices and patient outcomes.
Additionally, the center facilitates routine educational sessions and collaborative workshops, supporting professional growth among healthcare providers and progressively lifting industry norms.
A Future-Oriented Method in Orthopedics
As the landscape of orthopedic surgery transforms, Gough Surgical maintains its pioneering stance by regularly assimilating cutting-edge technologies and approaches.
The practice’s dedication to ongoing enhancement assures that individuals have access to state-of-the-art and highly effective therapies.
"{Our goal is to redefine what's possible in orthopedic surgery continually," affirms Dr. Gough.
"Innovation and patient care must evolve hand-in-hand," remarks further, Dr. Gough.
Final Thoughts: Leading the Way in Hip & Knee Treatment
Gough Surgical Adult Hip & Knee serves as a symbol of superior orthopedic treatment by combining state-of-the-art surgical methods, focused expertise, and heartfelt patient interaction.
By persistently surpassing traditional limits, Dr. James Gough and his focused team not only reestablish joint mobility—they dramatically enhance lives.
In the drive for freedom from pain and reenergized living, Gough Surgical Adult Hip & Knee goes beyond modifying orthopedic norms—it sets pioneering standards for tomorrow's healthcare.
Micro-Invasive together with Fiber-Preserving Operative Procedures: Evolving Modern Medicine
In recent decades, surgical innovation has redefined patient care, promising reduced trauma, brisk healing, plus augmented results.
Among these improvements, micro-invasive and muscle-maintaining strategies have surfaced as pioneering approaches.
These techniques have not only remodeled the operating room, but also redefined the patient experience.
This article surveys the evolution, techniques, benefits, challenges, and future directions in micro-invasive and fiber-preserving procedures, based on professional analyses, clinical evaluations, and pragmatic applications.
A Cutting-Edge Phase in Surgery: The Upsurge of Minimally Disruptive Methods
The modern intervention suite is a far cry from the large incisions and extended hospital stays that characterized surgery a century ago.
Modern-day surgeons increasingly rely on techniques that minimize tissue disruption and preserve the natural anatomy of the body.
Fundamental to these breakthroughs are characterized by micro-invasive and muscle-sparing methods.
Micro-invasive surgery refers to techniques that use small incisions, specialized instruments, and high-definition imaging to access and treat internal conditions with minimal disruption to surrounding tissues.
In contrast, muscle-sparing surgery focuses on preserving the integrity of muscle tissue during procedures that traditionally required more extensive muscle dissection.
Each technique contributes to a larger trend aimed at lowering patient morbidity, discomfort, and convalescence duration.
A Look Back: Transitioning from Open Surgery to Tissue Preservation
Surgical practices have long been dictated by necessity and available technology.
Before the breakthrough of current imaging and specialized instrumentation, clinicians resorted to large incisions to secure the necessary exposure for surgery.
While crucial for survival, these approaches often imposed marked postoperative pain, drawn-out recoveries, and risks of complications such as infectious issues or chronic muscle debilitation.
The shift took root with the advent of laparoscopic surgery in the late twentieth century—a minimally disruptive method that enabled internal visualization by inserting a tiny camera through small incisions.
As technology advanced, surgeons began to appreciate that preserving muscle integrity during procedures could offer even greater benefits.
tactics for sparing muscle tissue, initially designed for orthopedics and cardiovascular surgery, promptly found use in abdominal, gynecological, and oncological procedures, among additional specialties.
Dr. Eleanor Matthews , a pioneer in minimally invasive approaches at a respected teaching hospital, affirms: “We realized that every incision we made, every muscle we cut, had a lasting impact on our patients. The drive to improve quality of life post-surgery has pushed us to continually refine our methods.”
This shift toward less invasive techniques stands as both a technical feat and a profound change in the approach to surgical care.
The Science Behind the Techniques
Micro-Invasive Surgery: Precision Through Technology
Fundamental to micro-invasive procedures is the commitment to precision.
Surgeons use an array of high-tech tools—from endoscopes and robotic-assisted devices to specialized microscopes—to navigate the human body through minuscule openings.
These instruments grant high-level magnification and brightness, enabling meticulous identification and management of the target area with negligible tissue disruption.
One of the foremost advancements has been the blending of robotic-assisted surgical systems into practice.
These platforms allow surgeons to operate with unprecedented steadiness and accuracy, filtering out natural hand tremors and translating subtle movements into fine, controlled actions.
In operations like prostatectomies and cardiac procedures, such precision directly yields enhanced patient outcomes.
Heart and Thoracic Surgery: Minimizing Cardiac Trauma
Cardiothoracic procedures have markedly profited from minimally invasive techniques.
Methods such as valve repairs and CABG have generally called for substantial incisions and thorough muscle dissection.
Today, surgeons increasingly employ minimally invasive techniques that use small incisions and specialized instruments to access the heart and surrounding structures.
The adoption of robotic-assisted systems in cardiothoracic surgery has further refined these procedures.
In many cases, the robotic platform provides the precision required to perform delicate maneuvers on the beating heart, reducing the risk of complications and promoting faster recovery.
A comparative study published in the Annals of Thoracic Surgery found that patients undergoing minimally invasive valve repairs had lower rates of postoperative atrial fibrillation and shorter hospital stays compared to those who underwent conventional surgery.
General and Gynecologic Procedures: Improving Patient Results.
Within general and gynecologic practices, minimally invasive methods have transformed interventions like gallbladder removals, hernia repairs, and hysterectomies.
This transition to limited incisions and muscle conservation not only diminishes visible scarring but also lessens postoperative pain and the likelihood of complications.
As an illustration, laparoscopic cholecystectomy, which entails removing the gallbladder through tiny incisions, is now the standard treatment in many regions.
Patients benefit from shorter recovery times and the ability to resume normal activities almost immediately after the procedure.
In gynecology, muscle-sparing techniques have been instrumental in improving outcomes for women undergoing complex procedures such as myomectomies or pelvic floor repairs.
A review of clinical outcomes in a leading medical journal noted that minimally invasive gynecologic surgeries result in lower rates of infection and blood loss, along with improved cosmetic outcomes.
Such improvements both boost patient satisfaction and lead to superior overall health outcomes.
Weighing the Benefits and Challenges.
Benefits That Extend Beyond the Operating Room.
The gains from minimally invasive and muscle-sparing approaches extend far beyond the technical realm of surgery.
For patients, the benefits are tangible and life-changing.
The reduction in pain, scarring, and recovery time directly translates into a better quality of life.
In many cases, patients can return to work and resume daily activities within days rather than weeks, a critical factor in an increasingly fast-paced world.
From a comprehensive healthcare viewpoint, such techniques reduce overall hospital costs by minimizing both the length of stay and the postoperative care needed.
Additionally, fewer complications mean fewer readmissions, which is a significant consideration for healthcare providers and insurers alike.
The psychological benefits should not be underestimated.
Understanding that a surgery can be conducted with little bodily impact offers comfort and lowers preoperative stress.
This element is particularly significant for those facing extensive surgeries, with a calmer and positive perspective aiding better overall outcomes.
Obstacles and Limitations: A Pragmatic View.
Despite the numerous advantages, micro-invasive and muscle-sparing techniques are not without challenges.
One significant limitation is the steep learning curve associated with these advanced methods.
Surgeons need to complete comprehensive training and acquire significant experience to perform these techniques as proficiently as traditional methods.
High initial costs for advanced technology and training may restrict accessibility in resource-constrained areas.
Also, these approaches are not universally applicable to all patients.
For cases marked by extensive pathology or complex anatomy, the traditional open approach may be preferable and safer.
Surgeons are required to carefully analyze every situation, comparing the benefits of minimally invasive approaches with the patient’s individual circumstances.
Furthermore, inherent technical limitations can affect outcomes.
Despite the best state-of-the-art equipment, there are situations in which the operative field is constrained or unexpected issues emerge, forcing a switch to open procedures.
Even though such scenarios are rare, they illustrate the importance of maintaining a dynamic surgical team that can respond to unexpected challenges.
Expert Insights and Patient Perspectives
Testimonials from the Frontline
Dr. Michael Andersen, a well-respected surgeon with 25+ years of experience in minimally invasive methods, highlights the necessity of individualized treatment
“Every individual is unique, and while minimally invasive and muscle-conserving techniques deliver remarkable benefits, the crucial point is to adapt the approach to the patient’s particular clinical status and comprehensive health,” he explains.
His insights underscore a fundamental tenet of modern medicine: technology must serve the patient, not dictate the treatment plan.
Correspondingly, those who have undergone these procedures often express how these techniques have radically improved their quality of life.
Maria Lopez, a 54-year-old woman who recently underwent a muscle-sparing breast reconstruction, describes her journey.
“I anticipated a prolonged, painful recovery, but in reality, I was up and mobile within days, as if life had offered me a new beginning,” she explains.
Such individual accounts, despite being anecdotal, find support in robust clinical research showing enhanced outcomes with great post to read these techniques.
Establishing an Enduring Surgical Ecosystem.
The growing popularity of micro-invasive and muscle-sparing methods is fostering a broader cultural shift in healthcare.
Surgeons, medical centers, and training programs are increasingly partnering to exchange best practices, develop standardized procedures, and invest in ongoing research.
Regularly organized conferences and symposiums on minimally invasive techniques now serve as vital forums for expert discussion on innovations, obstacles, and future prospects.
A collaborative strategy is indispensable for resolving the difficulties that accompany these modern methods.
Through the collective sharing of expertise and resources, healthcare professionals are more capable of perfecting surgical methods, minimizing complications, and extending these benefits to a broader patient base.
The Evolution of Surgery: Trends, Technological Innovations, and Future Prospects.
Utilizing Artificial Intelligence and Advanced Robotics.
While current micro-invasive and muscle-sparing techniques have already made a profound impact, the future promises even more dramatic changes.
The integration of artificial intelligence (AI) and machine learning into surgical systems is poised to further enhance precision and efficiency.
Such systems can evaluate large datasets in real time, providing surgeons with predictive insights to optimize decision-making during sophisticated procedures.
For instance, AI-enabled imaging platforms are in development to automatically emphasize critical anatomical features, reducing the likelihood of accidental injury.
Robotic platforms are also evolving, with next-generation systems offering even finer control and enhanced haptic feedback, which allows surgeons to "feel" the tissue they are operating on—a feature that traditional laparoscopic instruments lack.
Expanding the Boundaries of Minimally Invasive Surgery.
Research and development in the field of tissue engineering and regenerative medicine are likely to intersect with surgical innovations.
Scientists are exploring ways to not only minimize tissue damage but also promote faster, more natural healing.
This includes the use of bioengineered scaffolds that can support tissue regeneration and reduce scar formation after surgery.
Moreover, as imaging and sensor technology continue to improve, surgeons may be able to perform procedures that are even less invasive than those currently available.
Innovations such as nanorobots and miniature, implantable devices could one day allow for targeted therapy and diagnostics at a cellular level, ushering in a new era of truly personalized medicine.
A Worldwide Perspective: Connecting the Gaps in Advanced Surgical Care
Even as next-generation technological solutions overhaul surgical methods in industrialized countries, pronounced inequities in accessing high-level surgical care are evident across the globe
Overcoming these disparities requires coordinated actions by state authorities, charitable organizations, and the global medical community
Training initiatives, technology exchange projects, and collaborative research ventures are crucial for ensuring that individuals worldwide benefit from innovations in minimally invasive and muscle-preserving surgery
Cross-border partnerships are demonstrating early signs of success
Hospitals in economically advanced countries are partnering with healthcare centers in less-developed regions to deliver education and aid in advanced minimally invasive methods
Such joint initiatives not only improve patient well-being but also promote the creation of a more balanced and accessible global health network
Steering Toward the Future: Challenges and Opportunities
The journey toward broad acceptance of minimally invasive and muscle-preserving surgical techniques is replete with challenges
The investment in cutting-edge equipment and specialized educational programs is often considerable
Still, the lasting improvements in treatment outcomes and healthcare cost efficiencies demonstrate that these difficulties are manageable
Policy makers and healthcare executives are increasingly recognizing that investments in advanced surgical tools can yield significant dividends
Abbreviated hospitalizations, reduced complication rates, and an expedited return to normal activities not only enhance patient well-being but also support a more effective and enduring healthcare structure
Accordingly, state agencies and commercial entities are increasingly committing resources to promote the innovation and distribution of these surgical methods
Moreover, the prevailing ethos within the surgical community is evolving
A focus on lifelong learning, interdisciplinary collaboration, and evidence-based practices is cultivating an atmosphere where innovation is both fostered and anticipated.
This cultural revolution is projected to speed up the acceptance of innovative practices and modern technologies, ultimately enhancing the quality of patient care worldwide.
Final Thoughts: A New Era of Patient-Focused Care.
The progression of micro-invasive and muscle-sparing interventions heralds a radical change in the operational model of surgical care.
These techniques have revolutionized the operating room by emphasizing precision, minimizing tissue trauma, and prioritizing muscle preservation, thereby improving patient outcomes and overall experience.
From the formative stages of laparoscopic surgery to today’s blend of robotics and AI, the pathway has been paved with constant innovation and a resolute drive for excellence.
For patients, the expected benefits include decreased pain, faster return to daily activities, and a higher level of life quality.
For surgeons and healthcare providers, the challenge is to master these innovative techniques, invest in cutting-edge technology, and cultivate a culture of constant advancement.
With the steady march of scientific research and technology, the potential for new innovations in these surgical techniques remains impressive.
Future surgical paradigms will focus on patient-centric care, with devices and procedures designed to improve, not impair, the body’s natural capabilities.
Looking forward, the synthesis of high-tech imaging, robotics, and regenerative medicine is expected to herald new frontiers in care that prioritize the patient.
The continual evolution of surgical techniques demonstrates the medical community’s steadfast commitment to innovation, ensuring safety, and striving for better outcomes.
As individualized healthcare becomes the norm, micro-invasive and muscle-sparing techniques emerge as symbols of a future where interventions are less traumatic and patient outcomes are significantly improved.
As our journey advances, every innovation brings us closer to a reality where surgery is not a precursor to pain and extended recovery but a stepping stone toward renewed health and vitality.
Further Documentation and References.
Clinical Studies and Reviews: Numerous scholarly articles in journals such as the Journal of Minimally Invasive Surgery, Annals of Thoracic Surgery, and the Journal of Surgical Education deliver extensive data on the benefits and outcomes of these surgical techniques.
Expert Interviews: Perspectives from expert surgeons, including Dr. Eleanor Matthews, Dr. Luis Hernandez, and Dr. Michael Andersen, provide detailed commentary on the practical challenges and advantages of micro-invasive and muscle-sparing procedures.
Technological Innovations: Recent progress in robotic-assisted procedures and the application of augmented reality in the OR are recorded in modern medical texts and presented at global surgical conferences.
These techniques have initiated a new phase in patient-focused surgical care. By concentrating on exact precision, minimizing trauma, and conserving muscle, they not only lead to better clinical outcomes but also significantly enhance the patient experience.
With ongoing technological advancements and broader adoption by the international medical community, the future of surgical care appears set to offer even greater benefits to patients across the globe.
Within this swiftly advancing domain, the dedication to constant improvement serves as the ultimate benchmark of progress—a pledge to revolutionize surgical care for years ahead.
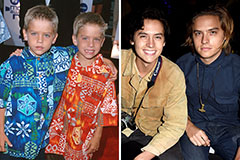 Dylan and Cole Sprouse Then & Now!
Dylan and Cole Sprouse Then & Now! Kelly McGillis Then & Now!
Kelly McGillis Then & Now! Barry Watson Then & Now!
Barry Watson Then & Now!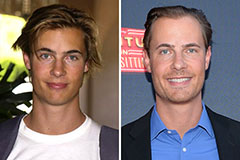 Erik von Detten Then & Now!
Erik von Detten Then & Now! Ryan Phillippe Then & Now!
Ryan Phillippe Then & Now!